Human Digestive System Definition
- The human digestive system is made up of the alimentary canal, several auxiliary organs, and a variety of digestive activities which occur at multiple stages in the digestive canal to prepare food taken in the diet for absorption.
- It has a fundamental structure that is modified on numerous different stages to account for the activities happening at every level.
- The breakdown of the intricate digestive processes of the consumed meals piece by piece until they are in a condition that can be absorbed.
- Nutrients are employed to synthesize parts of the body after absorption.
- These and other operations’ energy requirements, together with the waste materials removal, are provided by them. They also offer the essential ingredients for producing new cells, hormones, and enzymes.
- The gastrointestinal tract and auxiliary organs make up the human digestive system.
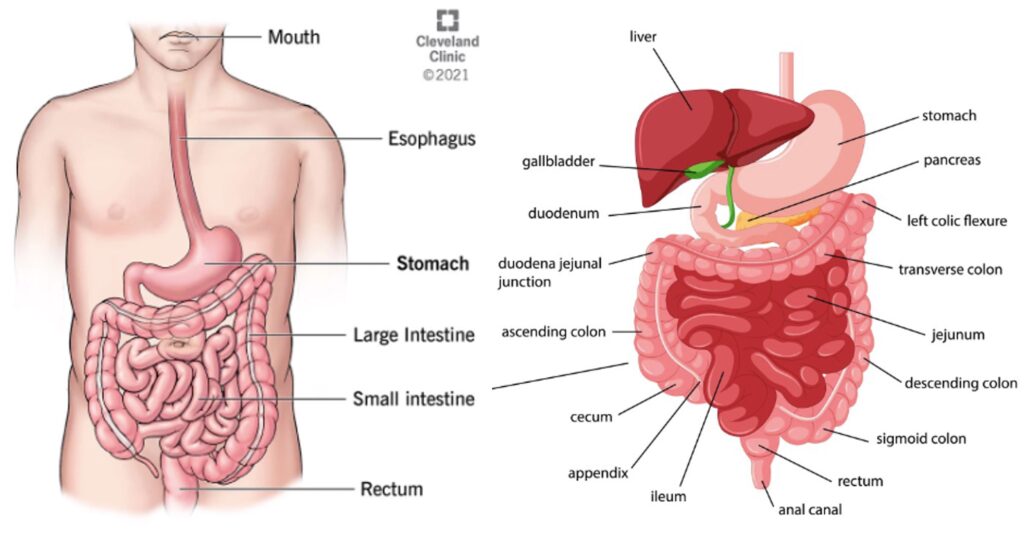
Alimentary Tract of The Human Digestive System
- Beginning at the mouth and continuing through the thorax, abdomen, and pelvis, the alimentary canal finishes at the anus. As a result, food travels via a lengthy tube. It has several components that are very similar structurally. The components are:
- Mouth
- Pharynx
- Oesophagus
- Stomach
- Small intestine
- Large intestine
- Rectum and Anal canal.
A. Mouth
- The lips, the oropharynx, the cheek muscles, the muscles of the hard and soft palates, the muscles of the tongue, as well as the soft tissues on the mouth’s floor, form the anterior and posterior borders of the mouth, the oral cavity, which is another name for it.
- It is completely covered by a mucous membrane, which has stratified squamous epithelium and microscopic glands that produce mucus.
- The anterior hard palate and the posterior soft palate make up the palate, which together comprises the roof of the mouth. The sides of the muscular soft palate integrate with the pharynx’s walls, and it slopes downward from the back of the hard palate.
- The center of the soft palate’s free border is where a muscle fold known as the uvula hangs down from and is coated in the mucous membrane.
- It consists of the following essential parts:
The Tongue
- The floor of the mouth is occupied by the tongue; a muscular tissue used voluntarily.
- It is joined to the hyoid bone at the base and the mouth floor at the frenulum, a fold in the mucous membrane covering.
- The superior surface comprises stratified squamous epithelium with many papillae, or small projections, that contain taste nerve terminals, also known as taste buds.
- The tongue has a crucial role in
- mastication (chewing)
- deglutition (swallowing)
- speech
- taste
The Teeth
- The sockets, or alveoli, of the mandibular and maxillary alveolar ridges, are where the teeth are located.
- Both temporary or deciduous teeth and permanent teeth are present in every person.
- Both dentitions teeth are present in the jaw and maxilla at birth in an immature state.
- The temporary teeth total 20, with 10 in each jaw. They start to appear at around six months, and by 24 months, they should all be present.
- The replacement of the deciduous teeth by the permanent ones starts in the sixth year of life, and the 32 teeth that make up this dentition are typically all present by the 24th.
Types and Functions of the Teeth
- In contrast to the premolar and molar teeth, which have a wide, the incisor and canine teeth are the cutting teeth utilized for biting off pieces of food. The teeth have flat surfaces and are utilized for grinding or chewing food.
B. The Pharynx
- Food travels from the mouth cavity via the pharynx and into the continuous esophagus below.
- The nasopharynx, oropharynx, and laryngopharynx are the three sections of the pharynx that are used for descriptive reasons.
- The nasopharynx is crucial for breathing. The respiratory and digestive systems share channels called the oropharynx and laryngopharynx.
Function of Pharynx
- The pharynx may be considered where the respiratory and digestive systems divide since they perform both functions.
- The muscle walls of the digestive tract play a role in swallowing and act as a conduit for the passage of food from the mouth to the esophagus.
- Peristalsis is greatly influenced by the constrictive circular muscles of the pharynx’s outer layer. Food and liquids that have been consumed will be securely transported through the digestive system by a sequence of contractions.
- However, the longitudinal muscles of the inner layer will broaden the pharynx laterally and elevate it upward, enabling the swallowing of ingested food and liquids.
C. The Oesophagus
- The esophagus is located in the middle plane of the thorax, in front of the vertebral column, behind the heart and the trachea, and is around 25 cm in length and 2 cm in width.
- It is continuous with the pharynx above, joining the stomach right below the diaphragm.
- Sphincter muscles seal the esophagus’s upper and lower ends.
- When you breathe in and aspirate oesophageal contents, the upper cricopharyngeal sphincter stops air from entering your esophagus.
- The cardiac sphincter sometimes referred to as the lower oesophageal sphincter, stops the reflux of acidic stomach contents into the esophagus.
Functions of Oesophagus
- Food and liquids go from the mouth to the stomach through the esophagus. Contractions that occur periodically achieve this (peristalsis).
- The esophagus is a vital conduit from the thoracic chamber, which safeguards the heart and lungs, to the digestive system.
- The esophagus’s two sphincters divide food into boluses, which are discrete portions.
D. The Stomach
- The abdominal cavity’s epigastric, umbilical, and left hypochondriac areas include the stomach, a J-shaped dilated segment of the alimentary system.
- The cardiac and pyloric sphincters connect the stomach to the esophagus and the duodenum.
- There are two curves in it. The shorter the rear surface of the stomach, the weaker curvature continues the posterior wall of the esophagus downward. It curls upward just before the pyloric sphincter to complete the J form.
- The anterior area bends sharply upward where the esophagus enters the stomach, curves downward to produce the larger curvature, and then gently angles upward toward the pyloric sphincter.
- The fundus, body, and antrum are the three sections of the stomach.
- The pyloric sphincter, which protects the passage between the stomach and the duodenum, is located at the distal end of the pyloric antrum.
- The amount of food that can fit in an adult’s stomach, which might be 1.5 liters or more, determines the size of the stomach.
- When the stomach’s gastric muscles contract, the bolus is broken down and mixed with gastric juice while peristaltic waves push the stomach’s contents toward the pylorus.
- Special secretory glands in the mucosa secrete around 2 liters of gastric juice daily.
- It comprises water, mineral salts, mucus produced by goblet cells on the stomach’s surface and in glands, hydrochloric acid, intrinsic factor, inactive enzyme precursors, etc.
Functions of the Stomach
- Temporary storage gives pepsins, the digesting enzymes, time to work.
- Pepsins chemically break down proteins to create polypeptides.
- Mechanical breakdown: The stomach’s three layers of smooth muscles allow it to churn when gastric juice is introduced, liquefying the contents to produce a chiming sound.
- performs restricted water, alcohol, and some lipid-soluble medication absorption.
- Gastric juice’s hydrochloric acid acts as a general defense against microorganisms.
- Getting ready for iron absorption later down the line—the stomach’s acidic environment solubilizes iron salts, which is necessary before iron can be absorbed.
- The terminal ileum produces the intrinsic factor required for vitamin B12 absorption.
- control over the duodenum’s entry of gastric contents. The pyloric antrum causes tiny jets of gastric contents to pass over the pyloric sphincter and into the duodenum when the chyme is sufficiently acidified and liquefied.
E. The Small Intestine
- At the pyloric sphincter, the small intestine joins the stomach, and at the ileocaecal valve, it enters the large intestine.
- It is a little over 5 meters long and is encircled by the big intestine in the abdominal cavity.
- Most of the nutritional absorption and the chemical breakdown of food occur in the small intestine.
- The small intestine is divided into three portions that run parallel to one another.
- Duodenum: The duodenum is approximately 25 cm long and curved around the pancreatic head. The hepatopancreatic ampulla, a structure shared by the gall bladder and pancreas that releases its secretions into the duodenum, is protected by the hepatopancreatic sphincter (of Oddi).
- Jejunum: The small intestine’s jejunum, roughly 2 meters long, is located in the center of the organ.
- Ileum: The ileocaecal valve controls how food moves from the ileum to the caecum, the first section of the large intestine, and it also helps to avoid regurgitation. It is located near the end of the ileum, or terminal region, which is around 3 meters long.
- Permanent circular folds, villi, and microvilli significantly enhance the surface area of the small intestinal mucosa.
- About 0.5 to 1 mm long, the villi are little, finger-like protrusions of the mucosal layer into the intestinal lumen.
- Their walls are made of enterocytes, which are columnar epithelial cells with minuscule microvilli (1 m long) on their free borders.
Functions of Small Intestine
- 90% of food digestion and absorption occurs in the small intestine, with the remaining 10% happening in the stomach and large intestine.
- The main function of the small intestine is to acquire nutrients and minerals from food.
F. The Large Intestine
- It measures around 1.5 meters in length, starting in the right iliac fossa at the caecum and ending at the rectum and anal canal in the deep pelvis.
- Its lumen is larger than that of the small intestine. It makes an arch over the coils of the small intestine.
- The many portions of the colon are the caecum, ascending colon, transverse colon, descending colon, sigmoid colon, rectum, and anal canal.
The Caecum
- The beginning of the colon is this. It is a dilated region that has a blind end inferiorly and is continuous with the ascending colon superiorly.
- The ileocaecal valve emerges from the ileum just below the point where the two join.
- The vermiform appendix emerges from the caecum as a little tube that is closed at one end. It is typically 13 cm long, similar in structure to the colon’s walls, but includes more lymphoid tissue.
The Ascending Colon
- This travels upward from the caecum to the level of the liver, where it forms the transverse colon by abruptly bending to the left at the hepatic flexure.
The Transverse Colon
- The loop of the colon that passes via the abdominal cavity in front of the duodenum and stomach to the area of the spleen, in which it creates the splenic flexure and abruptly bends downward, makes up the descending colon.
The Descending Colon
- Then it turns toward the midline after passing through the left side of the abdominal cavity. The sigmoid colon is the term used for it after it reaches the real pelvis.
The Sigmoid Colon
- This section discusses the S-shaped pelvic curvature that descends to form the rectum.
G. The Rectum and The Anal Canal
- It is a 13 cm long, somewhat dilated portion of the colon. The anal canal is where it ends after emerging from the sigmoid colon.
- The anal canal connects the rectum to the outside of the body and measures just 3.8 cm in length in adults.
- The autonomic nervous system controls the internal sphincter, whereas the external sphincter, which is formed of skeletal muscle and controlled voluntarily, is composed of smooth muscle fibers.
Functions of Rectum, Anal Canal, and Large Intestine
Absorption
- The ileum’s contents flow through the ileocaecal valve and into the caecum as fluid, although little water has been collected in the small intestine.
- Water absorption in the large intestine continues until the feces’ well-known semisolid consistency is reached.
- The large intestine also absorbs vitamins, mineral salts, and certain medications into the blood capillaries.
Microbial Activity
- The big intestine is extensively populated by certain bacterial species that produce folate and vitamin K. They consist of Clostridium perfringens, Streptococcus faecalis, Enterobacter aerogenes, and Escherichia coli (welchii).
Defaecation
- Usually, the rectum is empty. A significant movement activates the nerve endings in its walls and forces the contents of the sigmoid colon into the rectum.
- The internal anal sphincter relaxes and the rectus muscle contracts uncontrollably during defecation.
- The Valsalva technique, which involves contracting the abdominal muscles and lowering the diaphragm, raises intra-abdominal pressure and facilitates defecation.
Accessory Organs of The Human Digestive System
- The alimentary canal receives a variety of secretions, some produced by glands in the lining membrane of the organs, such as the glands that produce gastric juice in the lining of the stomach and others by glands outside the tract.
- The latter is the digestive system’s auxiliary organs, and their secretions travel through ducts before reaching the tract. They include:
- Three sets of salivary glands
- Pancreas
- Biliary tract and the liver.
Physiological and anatomical connections exist between the organs and glands.
A. The Salivary Glands
- The oral cavity contains salivary glands that release their secretions into the mouth.
Saliva
The secretions of the salivary glands and the small glands are combined to form saliva that lines the mouth canal and secretes mucus. Each day, around 1.5 liters of saliva is generated, and it contains:
- water
- mineral salts
- salivary amylase is an enzyme.
- mucus
- lysozyme
- immunoglobulins
- blood-clotting factors.
- The parotid, submandibular, and sublingual glands are the three pairs.
Parotid Glands
- These are positioned slightly below the external auditory meatus on either side of the face, one on each side.
- The second upper molar tooth level is where the parotid ducts of each gland enter the mouth.
Submandibular Glands
- One of these is located under the angle of the jaw on each side of the face.
- One on either side of the tongue’s frenulum, the two submandibular ducts open on the floor of the mouth.
Sublingual Glands
- In front of the submandibular glands, these glands are located beneath the mucosal membrane of the oral cavity.
- They feature a large number of tiny ducts that exit into the mouth’s floor.
Functions of Salivary Glands and Saliva
- Chemical digestion of polysaccharides: Chemical polysaccharide digestion Amylase, an enzyme found in saliva, starts to break down complex sugars and transforms them into the disaccharide maltose.
- Lubrication of food: Food lubrication. Before becoming a bolus ready for swallowing, dry food that enters the mouth is moistened and lubricated by saliva.
- Cleansing and lubricating: lubricating and cleaning. An appropriate flow of saliva is required to keep the mouth’s tissues supple, moist, and malleable and clean the mouth. It aids in preventing abrasive or rough meals from harming the mucous membrane.
- Non-specific defense: unfocused defense. Invading bacteria are fought off by lysozyme, immunoglobulins, and clotting factors.
- Chemicals in solution are the only things that can excite the taste buds. Dry foods don’t actually activate the taste buds until they’ve been thoroughly mixed with saliva.
B. The Pancreas
- The pancreas is an approximately 60-gram gland with a light grey color.
- It is located in the left hypochondriac and epigastric areas of the body and is approximately 12 to 15 cm long.
- abdominal cavity.
- Its body, large head, and short tail are all present. The tail touches the spleen and is located in front of the left kidney. The body is behind the stomach, and the head is in the duodenal curve.
- Exocrine and endocrine glands both exist in the pancreas.
The Exocrine Pancreas
- It is made up of several lobules that are comprised of tiny alveoli and have secretory cells as their walls.
- The pancreatic duct, which is present throughout the gland and leads to the duodenum, connects the tiny ducts that drain each lobule at the end.
- The hepatopancreatic ampulla is formed when the pancreatic duct meets the common bile duct just before it enters the duodenum. The hepatopancreatic sphincter regulates the ampulla’s duodenal opening (of Oddi).
- The exocrine pancreas’ job is to secrete pancreatic juice, which contains enzymes that break down carbs, proteins, and lipids.
The Endocrine Pancreas
- The pancreatic islets are clusters of specialized cells dispersed throughout the gland (of Langerhans).
- The hormones diffuse straight into the circulation because the islets lack ducts.
- The endocrine pancreas secretes the hormones insulin and glucagon, which are principally responsible for regulating blood glucose levels.
You may also like to read: Stratified Cuboidal Epithelium
Functions of the Pancreas
- The pancreas, a part of the exocrine system, secretes enzymes that work in conjunction with bile from the liver and gallbladder to help break down food for the best possible digestion and absorption.
- The pancreas makes the following digestive enzymes:
- Lipase breaks down fats.
- carbohydrate digestion with amylase
- Use trypsin and chymotrypsin to break down proteins.
- Enzymes are created by the pancreas as soon as food reaches the stomach.
- Before reaching the major pancreatic duct, these enzymes pass through several ducts.
- The common bile duct, which transports bile from the liver and gallbladder to the duodenum, intersects the main pancreatic duct. The ampulla of Vater is the name of this gathering place.
- The pancreas pumps enzymes and bile from the gallbladder into the duodenum to assist in the metabolism of lipids, carbohydrates, and proteins so that they might be absorbed by the digestive system.
Endocrine Function
- The endocrine system organ known as the pancreas secretes two main hormones which are vital for regulating blood glucose levels:
- Insulin: This hormone is released by the pancreas to lower blood glucose levels if it becomes too high.
- Glucagon: The pancreas produces the hormone glucagon while blood glucose levels drop too low, which boosts blood glucose levels.
- The liver, kidneys, and brain benefit significantly from stable blood glucose levels. Your neural and cardiovascular systems, among other biological systems, depend on properly producing these hormones.
C. The Liver
- The liver, which weighs between 1 and 2.3 kg, is the biggest gland in the body.
- The upper abdominal cavity contains the bulk of the right hypochondriac region, a small piece of the epigastric region, and the left hypochondriac region.
- Its rear surface is uneven in shape, while the top and front surfaces of the diaphragm are smooth and curved to resemble the diaphragm’s underside.
- The peritoneum covering the liver is not complete, and the liver is surrounded by a thin, inelastic capsule. Assisting ligaments connecting the liver to the inferior surface of the diaphragm is formed by peritoneal folds. These ligaments and the abdominal cavity’s pressure from the organs work together to hold it in place in part.
- Four lobes make up the liver. The two which stand out the most are the enormous right lobe and the smaller, wedge-shaped left lobe. The components of the posterior surface that comprise the other two are the caudate and quadrate lobes.
- The liver’s lobes are made up of minute, hardly perceptible lobules.
- Hepatocytes, which have a cubic structure and are grouped into pairs of columns radiating from a central vein, produce the hexagonal-shaped lobules that make up the liver.
- There are sinusoids (blood channels with partial walls) in between two pairs of columns of cells that carry a combination of blood from the small branches of the portal vein and hepatic artery.
- Hepatic macrophages (Kupffer cells) have the job of ingesting. An additional function of the cells lining the sinusoids is to filter out any foreign chemicals in the blood that pass through the liver.
- The central or centrilobular veins receive blood that is released by the sinusoids. These eventually develop into the hepatic veins, which leave the liver and connect with veins from other lobules to form larger veins. These veins empty into the inferior vena cava just below the diaphragm.
Functions of the liver
- Secretion of bile. biliary secretion. In the sinusoids, the hepatocytes create the components of bile from mixed arterial and venous blood. These consist of cholesterol, bile salts, and bile pigments.
- Metabolism of carbohydrates: Insulin-induced conversion of glucose to glycogen and glucagon-induced conversion of liver glycogen back to glucose. The blood glucose level is significantly regulated by these changes.
- Metabolism of fat: The process involves the desaturation of fat or change of the form of stored fat so that it may be used as fuel by tissues.
- Protein metabolism.Deamination: protein synthesis. The nitrogenous component of amino acids not needed for synthesizing new protein is removed by deamination; this nitrogenous fraction is converted to urea, which is then expelled in the urine.
- Additionally, uric acid, which is expelled in the urine, is formed when the genetic material of the body’s worn-out cells is broken down.
- Transamination: This process separates the nitrogenous part of amino acids from other carbohydrate molecules to create new non-essential amino acids.
- The liver is where amino acids are converted into plasma proteins and most blood clotting factors.
- Destruction of erythrocytes and microbial defense: Phagocytic Kupffer cells (hepatic macrophages) in the sinusoids perform this.
- Detoxification of harmful chemicals and drugs: These include alcohol (ethanol) and microbe-produced poisons.
- ethanol metabolism.
- Hormone inactivation: These include sex hormones, thyroid, aldosterone, cortisol, glucagon, and insulin.
- Synthesis of vitamin A from carotene: vitamin A is created from beta-carotene. (Carotene, a provitamin, is present in some plants, such as carrots and the green leaves of various vegetables.)
- The creation of heat: The liver has a high metabolic rate, consumes a lot of energy, and generates a lot of heat. It is the primary organ of the body that produces heat. It takes part in storing A, D, E, and K fat-soluble vitamins, copper, and iron. There are a few water-soluble vitamins, including riboflavin and niacin, vitamin B12, folic acid, and pyridoxine.
References
- Stomach: clevelandclinic.org
- digestive system: cancer.gov





